I. Introduction
Telehealth is revolutionizing healthcare by enabling remote monitoring, diagnosis, and treatment. Integrating biometric technologies enhances security and personalization, with ECG biometrics standing out due to their uniqueness, resistance to spoofing, and continuous monitoring capabilities. Unlike fingerprints or facial recognition, ECG signals offer both secure authentication and real-time health tracking, making them ideal for telehealth applications where privacy and security are critical. Figure 1 outlines the key components of an ECG-based telehealth system, from data acquisition to health monitoring.
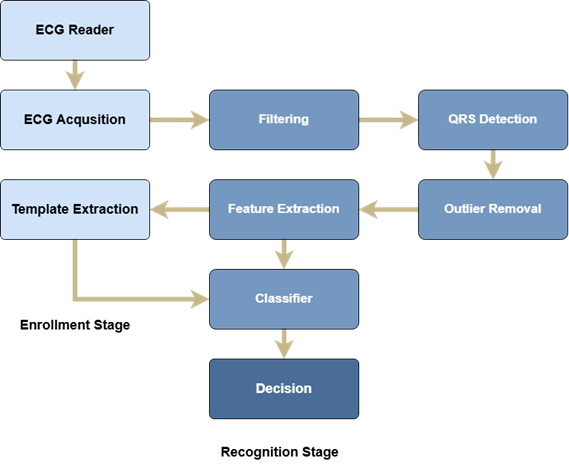
Fig. 1. Block diagram of a typical ECG biometric system
II. Why ECG biometrics
The uniqueness of ECG signals stems from the fact that they reflect the physiological and anatomical characteristics of an individual's heart. This makes them an ideal candidate for biometric identification and authentication. Additionally, ECG signals can only be captured from a living person, providing inherent liveness detection and making them resistant to spoofing attacks [1, p. 123-135]. Furthermore, ECG sensors integrated into wearable devices allow for non-intrusive and continuous monitoring, enabling simultaneous health tracking and authentication. For example, wearable devices such as smartwatches equipped with single-lead ECG sensors have demonstrated the potential for seamless integration into daily life [2, p. 2456-2467]. These advantages position ECG biometrics as a cornerstone technology for enhancing the security and functionality of telehealth systems.
III. Framework for using ECG biometrics in ECG
The implementation of ECG biometrics in telehealth applications involves several interconnected components. The first step is data acquisition, which relies on wearable devices such as smartwatches, chest straps, or patches. Proper sensor placement and a sufficient sampling rate are critical to ensure high-quality signal capture. Once acquired, the raw ECG signals undergo preprocessing to remove noise and artifacts. Techniques such as bandpass filtering, wavelet transforms, and baseline correction are commonly employed to enhance signal quality [3, p. 101829].
Following preprocessing, feature extraction is performed to identify distinctive patterns in the ECG signal. Temporal features like RR intervals, morphological features such as the QRS complex, and frequency domain features are extracted to create a biometric template. Advanced machine learning algorithms, including deep learning models, can automatically extract hierarchical features from raw ECG signals, improving accuracy and robustness [4, p. 156-168].
The next step involves authentication and identification, where the incoming ECG signal is compared with the stored template using similarity metrics such as Euclidean distance or dynamic time warping. A decision threshold determines whether the match is sufficient for authentication. Finally, the system integrates with telehealth platforms through secure data transmission protocols and cloud storage, enabling real-time health monitoring and alerts for healthcare providers. Figure 2 provides a detailed flowchart of the ECG biometric authentication process within a telehealth application.
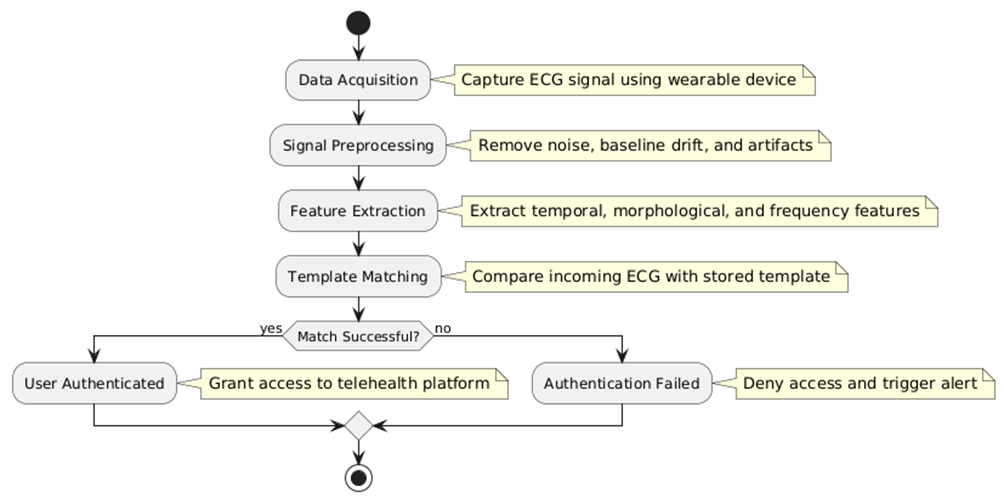
Fig. 2. ECG biometric authentication process
IV. Challenges and applications
Despite its potential, the deployment of ECG biometrics in telehealth faces several challenges. Signal variability due to factors such as stress, physical activity, and aging can affect authentication accuracy [5, p. 301-315]. Ensuring interoperability across different wearable devices and platforms is another critical consideration. Privacy concerns also arise, as sensitive health data must be protected against unauthorized access and breaches. Regulatory compliance with standards such as HIPAA (Health Insurance Portability and Accountability Act) or GDPR (General Data Protection Regulation) is essential for widespread adoption [6, p. 45-52]. Addressing these challenges requires a multidisciplinary approach involving advancements in signal processing, cybersecurity, and regulatory frameworks.
The integration of ECG biometrics in telehealth is still in its nascent stages, but ongoing research and technological advancements promise exciting possibilities. AI-driven analysis using deep learning and machine learning algorithms can improve feature extraction and classification accuracy, enabling more robust authentication systems [7, p. 102417]. Combining ECG with other biometric modalities, such as photoplethysmography (PPG) or voice recognition, can enhance security and reliability. Edge computing, where ECG data is processed locally on wearable devices, can reduce latency and improve privacy. Furthermore, continuous ECG monitoring can enable personalized medicine by facilitating tailored healthcare interventions based on individual health profiles.
V. Conclusion
ECG biometrics offer a powerful framework for enhancing telehealth applications by providing secure authentication and real-time health monitoring. By addressing current challenges and leveraging emerging technologies, ECG-based systems can revolutionize remote healthcare delivery. As wearable devices become more advanced and accessible, the adoption of ECG biometrics in telehealth is poised to grow, paving the way for a more connected, secure, and personalized healthcare ecosystem. Future research should focus on improving algorithm robustness, ensuring regulatory compliance, and exploring multimodal biometric systems to unlock the full potential of ECG biometrics in telehealth.
.png&w=384&q=75)
.png&w=640&q=75)